So that we may perform well the following day, getting a decent night’s sleep is essential. Even though sleep deprivation might make seizures more frequent, for some people with epilepsy it can also cause them to feel exhausted throughout the day.
- Top 10 Best Bamboo Pillow Reviews Update 06/2025
- Ultimate Guide to Choosing a Best Backpacking Quilt Update 06/2025
- How Does Sex Affect Sleep? Is Sex Before Sleep a Good Thing? Update 06/2025
- Why Do I Need A CPAP Prescription? How Do You Get a CPAP Prescription? Update 06/2025
- Top 6 Best Camping Pillows on Amazon Update 06/2025
Are there links between epilepsy and sleep?
Epilepsy and sleep are intertwined in a myriad of ways. The brain is active while we sleep, digesting information that aids our cognitive development. Throughout the course of a night’s sleep, the brain undergoes many stages of activity.
Bạn đang xem: Sleep and Epilepsy: How Can I Help Improve My Sleep? Update 06/2025
Different stages of sleep
The two types of sleep, which alternate in frequency and duration, occur in an alternating pattern.
- Stages of light, non-rapid eye movement (NREM), and deep sleep.
- sleeping with rapid eye movement (REM)
Non-rapid eye movement sleep
Light sleep
- Our muscles begin to relax in the first stage of non-rapid eye movement (NREM) sleep, which is characterized by a state of wakefulness that is somewhere between alertness and slumber.
- People with epilepsy are more likely to have seizures during stage two of sleep because their heart rate and respiration drop down during this stage.
Deep sleep
- Stage three is a profound slumber (sometimes called slow-wave sleep). Our breathing and pulse rate drop-down and our brain produces ‘delta waves,’ a type of brainwave associated with deep sleep.
- It becomes increasingly difficult to be roused from a deep slumber as delta waves rise. Many of us will be bewildered if we are woken up at this stage. Deep sleep is when sleepwalking and night terrors are more common than light sleep.
NREM sleep is thought by scientists to be critical to the development of long-term memories and the strengthening of connections between brain cells during sleep. In addition to aiding the body’s recovery from the day’s activities, a good night’s sleep also aids the brain in its own recovery.

Rapid eye movement sleep
The most vivid dreams come during the third stage of profound sleep. It’s at this stage of sleep that the brain is trying to organize all the information it’s gathered during the day.
Uncertainty surrounds the function of rapid eye movement (REM) sleep and dreams. Theoretically, this may help us make sense of our thoughts and ideas, as well as our feelings and memories associated with them.
Memory and judgment might be harmed by a lack of sleep. It has the potential to have an impact on our emotions as well as our immune system.
Are there links between seizures and sleep?
Having a hard time sleeping can be a cause for seizures in some people, for example. Seizures can occur as soon as a person wakes up or within the next several hours in some types of epilepsy. Seizures can impair sleep at any time of the night, and seizures during the day might affect the next night’s sleep for those with epilepsy who have an irregular sleep pattern. Seizures can disrupt sleep patterns for up to a week or more for some people.
Do antiepileptic drugs affect sleep?
Some patients may experience side effects with anti-epileptic drugs (AEDs), just like with any other medication. It is possible that AEDs can have varying effects on sleep, depending on the dosage. As sedatives, certain AEDs have the potential to make patients feel drowsy. Sleep disorders such as insomnia and sleep apnea have been linked to some of these medications. Some AEDs, on the other hand, have been shown to improve sleep quality by lengthening the period of deep sleep.
Seizures that start during sleep
The term “asleep seizure” (also referred to as “nocturnal seizures”) refers to a type of seizure that occurs when a person is asleep, either as they are falling asleep or waking up. Seizures in the frontal lobe of the brain can occur both during non-rapid eye movement (NREM) sleep and when the patient is awake. Seizures in the frontal lobe frequently occur in ‘clusters,’ but are usually brief. Insomniac wandering and jerking, unusual arm and leg postures and motions, and shrill screaming are all examples of these symptoms.
Sleep disorders
‘Parasomnias,’ or sleep-related anomalies, are a specific type of sleep disorder. These include, but are not limited to, sleep paralysis, sleepwalking, and night terrors (where a person suddenly wakes from sleep in a state of panic or fright). Some areas of the brain may be awake while others are asleep, resulting in this condition. In some parasomnias, you may find yourself producing strange noises or motions. At times, determining whether someone is experiencing seizures or parasomnia might be challenging. To aid in the process of diagnosis, having a written or video record of what transpires during the incident can be beneficial. In many cases, the beginning and end of a seizure may be distinguished from one another because they follow a consistent pattern. Parasomnias, on the other hand, don’t always follow a set pattern and often don’t terminate. Neuralgias (uncontrollable desires to sleep at any moment of the day) might be mistaken for epilepsy in some cases. Some persons with narcolepsy, for example, suffer from cataplexy, a loss of muscle tone that affects the jaw, neck, and limbs, among other areas. Slurred speech and blurry vision can also be signs of a seizure. These emotions, such as laughing, wrath, and surprise can cause a person to have cataplexy.
Epilepsy and sleep disorders
Some medical illnesses, such as sleep disturbances, might be mistaken for epilepsy in patients with the condition. The occurrence of epilepsy is associated with an increased risk of OSA, which occurs when people snore and then cease breathing for short periods of time while they are asleep. Low muscle tone in the area of the airway can be a contributing factor. This could be due to the fact that some AEDs can cause weight gain as a side effect. Some persons with obstructive sleep apnoea may experience convulsions. An easy, painless test to monitor oxygen levels in your blood overnight can help diagnose obstructive sleep apnea if you snore and are told you stop breathing while sleeping by your doctor. Sleep-apnoea-trust.org provides information and a list of NHS sleep clinics in the United Kingdom that can help.

Tips for getting good sleep
You may be able to improve your quality of sleep by following a few simple guidelines.
Try a milky beverage instead of a caffeinated beverage if you generally have a hot drink before bedtime (research suggests that reducing caffeine up to six hours before bed can increase the quality of sleep).
Avoid late-night suppers and alcoholic beverages, if at all possible.
Set a regular bedtime and a regular wake-up time.
Keeping mobile devices like smartphones and tablets out of the bedroom will help you get a good night’s sleep.
Prevent watching television or using a computer right before going to bed.
Keep your room at a reasonable temperature and as dark as possible to create a peaceful atmosphere.
Xem thêm : Top 10 Best Bamboo Pillow Reviews Update 06/2025
To get a good night’s sleep, make sure your mattress and pillow are both comfy.
Napping should be limited to 15 minutes or less at any given time of day. This can help you sleep more regularly at night.
You can get referred to a specialist sleep clinic by your doctor or consultant if you are having trouble sleeping.
To Dr. Hugh Selsick, of the Royal London Hospital for Integrated Medicine, we owe our thanks for his assistance in compiling this data.
Epilepsy and the Brain
Electrical impulses transmit information between the nerve cells that make up the brain. Neurotransmitters are chemical messengers that carry these impulses throughout the body. The brain’s electrical activity is generally well-controlled.
The brain’s electrical activity and connections become abnormal in persons with epilepsy, resulting in abrupt bursts of electrical impulses that alter a person’s thoughts, feelings, and behaviors. Numerous epilepsy syndromes and forms exist.
Epilepsy and Sleep
Epileptic seizures and disturbed sleep have long been linked in the minds of medical professionals. When Aristotle first noticed this relationship, doctors in the late 19th century realized that most nocturnal seizures occurred during the time when a person went to sleep and woke up.
Sleep and epilepsy are linked in numerous ways by researchers. The impact of sleep on seizure timing and frequency is still being studied and is an important diagnostic tool for epilepsy.
Diagnosing Epilepsy
When two or more unprovoked seizures occur at least 24 hours apart, doctors consider a diagnosis of epilepsy. While medical illnesses, brain injuries, aberrant brain development, or an inherited genetic issue may all be to blame for epileptic seizures, this isn’t always the case.
An electroencephalogram (EEG) is one of the tools a neurologist uses to evaluate a seizure patient (EEG). When abnormal electrical activity is detected and located, EEGs help doctors determine if the abnormal activity is occurring from all over the brain or only from a specific area. Epileptiform abnormalities are patterns of aberrant brain activity that neurologists seek on EEGs. Spikes, sharp waves, and spike-wave patterns are all examples of these aberrant brain waves.
Particularly during the non-rapid eye movement (NREM) stage of sleep, anomalies in epilepsy are more likely to develop. An EEG may be performed while the patient sleeps in order to maximize the chances of detecting anomalies in the brain’s electrical system.

Epileptic Seizures While Sleeping
At any hour of the day or night, epileptic seizures can occur. Approximately 20% of patients with epilepsy have seizures only when they sleep, while 40% have episodes while awake, and 35% have seizures both while awake and asleep.
During non-rapid eye movement (NREM) sleep, electrical activity in different parts of the brain may be synchronized, which may be linked to seizure activity. Seizures can be caused by too much or too much synchronization. Another theory suggests that circadian rhythms and melatonin synthesis may be to blame.
In a number of different types of epilepsy, seizures can happen while you’re asleep.
- Nocturnal frontal lobe epilepsy (NFLE): The vast majority of NFLE sufferers experience seizures during non-rapid eye movement (NREM) sleep. At any age, however, it is more frequent in children, this syndrome can arise. People with NFLE may not be aware of their nightly seizure activity when they wake up in the morning.
- Benign epilepsy with centrotemporal spikes (BECTS): In children, BECTS is the most frequent kind of epilepsy, and it often begins between the ages of 3 and 13. 70 percent of the seizures in children with this type of epilepsy occur when they are sleeping, frequently just as they are about to drift off to sleep or as they are about to get up in the morning.
- Panayiotopoulos syndrome: Between the ages of 3 and 6, this type of epilepsy is most common. Sleeping seizures account for 70% of all seizures, with the remaining 13% occurring when the child wakes up. However, most children with this syndrome have fewer than five seizures before they are put on the road to recovery.
Epilepsy with continuous spike-waves in sleep and Lennox-Gastaut syndrome are three more sleep-related epilepsies that can be inherited (CSWS).
Epilepsy and Sleep Deprivation
People with epilepsy must make sure they get enough sleep each night. This association isn’t universal, but people with epilepsy are more likely to have seizures if they don’t get enough sleep, even if they don’t have a history of seizures.
Neuronal excitability is one theory as to why sleep deprivation might cause seizures. Undersleeping increases the likelihood of substantial fluctuations in electrical activity in the brain’s neurons. A seizure may be triggered by aberrant electrical activity in the brain of someone with epilepsy.
Epilepsy and Sleep Disorders
For both mental and physical well-being, sleep is essential. People with epilepsy are more likely to suffer from sleep difficulties. Epilepsy is thought to be a contributing factor in a variety of sleep problems.
- Insomnia: It is not uncommon for patients with epilepsy to suffer from sleeplessness, with a prevalence of between 24% and 55%. Seizures during the night, medications and the impacts of worry and sadness can all contribute to insomnia in people with epilepsy.
- Obstructive sleep apnea: OSA, or obstructive sleep apnea, is a sleep-related breathing disease in which the upper airway partially or completely collapses. OSA is twice as common among epilepsy patients as it is in the general population, affecting up to 30% of those who suffer from it. Snoring, frequent awakenings and difficulty sleeping can all be symptoms of sleep apnea.
Parasomnias are sleep disorders that include peculiar actions that take place before, during, and after sleep. NREM-related parasomnias, REM-related parasomnias, and other parasomnias are the three main types of parasomnias.
Scientists are still trying to figure out how parasomnias and epilepsy are connected. Many patients with epilepsy are also diagnosed with parasomnias since it can be difficult to tell the difference between epilepsy and parasomnias.
- NREM-related parasomnias: There are a number of conditions that fall under this umbrella. There are some forms of epilepsy that can be difficult to distinguish from sleep problems, such as nocturnal frontal lobe epilepsy. Some patients have arousal issues in their family history, which further complicates the distinction between nighttime and daytime seizures.
- REM-related parasomnias: Violations and unexpected bodily movements are among the symptoms associated with REM sleep behavior disorder. As many as 12% of older adults with epilepsy may have this illness undetected.
Epilepsy and Children
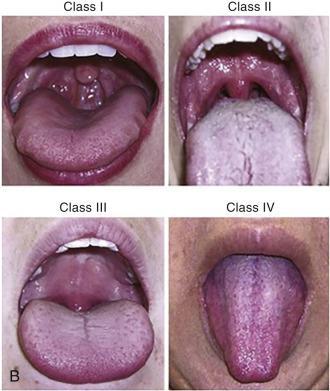
Xem thêm : Mallampati Score to Help Predict Obstructive Sleep Apnea Update 06/2025
As a child, you are in the midst of a period of rapid change and development. A child’s development, learning, and memory are all impacted by sleep, so getting enough of it is critical throughout this period.
Children with epilepsy are more likely to have sleep problems. Children with epilepsy, when compared to their unaffected siblings, were shown to have higher sleep disturbances and increased daytime sleepiness, according to studies.
Epilepsy patients need to take care of their sleep issues in order to function at their best. 30 to 60 percent of children with epilepsy have sleep-related breathing abnormalities including OSA, and parasomnias are widespread in some kinds of childhood epilepsy.
Children with epilepsy are still being examined for ways to enhance their sleep, but researchers have found that parent-based therapies can help children with other diseases that influence their sleep as well. In order to lessen seizures and limit long-term problems, parents of children with epilepsy can benefit from discussing treatment options with the child’s medical team.
Managing Epilepsy
Many people’s seizures can be reduced or eliminated with epilepsy treatment. Anticonvulsants or antiepileptic medicines are the most usually prescribed course of action. Surgery and vagus nerve stimulation are two further treatment alternatives if medicine does not control seizures effectively enough.
Lifestyle adjustments can assist people who have been diagnosed with epilepsy in better managing their health and potentially lessen their frequency of seizures. Self-management techniques, such as obtaining enough sleep and altering one’s diet, can be beneficial in the treatment of epilepsy.
Medications and Epilepsy
Antiepileptic drugs can have an impact on sleep, but it can be difficult to tell if this is due to the medication or the physical and social impacts of epilepsy. These drugs have a wide range of possible side effects. Some drugs can make you sleepy, while others can make you more awake.
Using antiepileptic medicines to treat sleep disorders may be an option for doctors. If a patient has insomnia, for example, doctors may prescribe antiepileptic medicines that promote sleepiness at nighttime. Patients who complain of excessive daytime sleepiness may be prescribed stimulant antiepileptic medications.
For many persons with epilepsy, a better night’s rest and reduced frequency of seizures may be possible with the use of sleep medications. Melatonin’s effect on sleep quality in patients with epilepsy has yet to be determined. If you have epilepsy and are considering taking a sleep aid, you should consult your doctor first.
Tips for Better Sleep
With epilepsy, sleep loss can have a negative impact on a person’s mood and quality of life. Excessive daytime sleepiness is a common complaint among those who suffer from epilepsy, in fact. As a result of the consequences of nocturnal seizures, antiepileptic drug side effects, and the stress and anxiety associated with controlling epilepsy and coping with social stigma, many persons with epilepsy have difficulty sleeping.
Epilepsy patients can benefit from open communication with their medical team about any sleep-related concerns they are encountering. A doctor can be a good source of information on several topics:
- Ask about sleep disorders: Your doctor may be able to help you better manage your epilepsy by diagnosing an undiscovered sleep issue. Epilepsy seizures can be cut in half by treating sleep problems like OSA.
- Talk about side effects of medications: If antiepileptic medications are functioning and if they have any unanticipated side effects, doctors need to know about them. Make sure to ask your doctor what side effects you can expect, and be sure to notify your doctor if you encounter any negative effects.
- Discuss stress and anxiety: Living with epilepsy can have a profound impact on a person’s quality of life and be taxing on the body and the mind. It’s quite natural to feel a wide range of emotions and for those feelings to shift. You may benefit from talking to a doctor, a support group, or a counselor about your emotions. Stress and worry can make it difficult to get a good night’s sleep, but by working with one of these professionals, you can get the aid you need.
People with epilepsy can benefit from improving their sleep hygiene while working with their medical team to address sleep difficulties. By concentrating on the habits that affect sleep, good sleep hygiene helps people get a good night’s sleep. The following are a few ideas to help you sleep better:
- Schedule your sleep: Consistent sleep patterns help you obtain the quantity of sleep you require. Even on the weekends, try to maintain a regular bedtime and wake time, even if it’s just for one night a week.
- Make a nightly routine: Preparing for bed by following a regular routine can help you fall asleep more quickly. For 30-60 minutes before going to bed, set a timer or a reminder on your phone or computer to turn off gadgets, dim the lights, and engage in some form of relaxation.
- Improve daytime habits: During the waking hours, our actions have a big impact on our sleep. Don’t drink alcohol, smoke cigarettes, or eat large meals before night, and get plenty of exercises and natural light during the day.
FAQs
Can Sleep Deprivation Trigger A Seizure?
It’s possible, yes. Seizures are highly reliant on a person’s sleep schedule. Getting their first and only seizure as a result of a college “all-nighter” or from a prolonged period of poor sleep is not uncommon. People with epilepsy are more prone to experience seizures if they don’t get “excellent sleep.” Even the strength and duration of seizures can be increased by using it. Those with certain types of epilepsy are more susceptible to sleep disturbances.

Why Does Sleep Deprivation Provoke Seizures?
Seizures can be effected in a variety of ways by sleep. Changes in the brain’s electrical and hormonal activity occur during regular sleep-wake cycles. Why some persons have more sleep-related seizures than others, as well as the connection between sleep deprivation and seizure occurrence, may be explained by these modifications. Seizures in certain persons are intimately linked to sleep. It is possible that they have all of their seizures while they are sleeping or waking up. However, for others, the link between insomnia and sleep may be less evident. Seizures, for example, maybe triggered only when other triggers are present.
What Causes Sleep Problems?
Seizures might be worsened if a person’s sleep is disrupted in any way. Here are some things to keep in mind.
- Not getting enough sleep: You don’t have to get the same amount of sleep like everyone else. Only 5 hours of sleep every night works for some people, while others require 8 to 10 hours or more. A decent night’s sleep is generally believed to be between seven and eight hours, but the quality of that sleep must also be taken into account. If people sleep less than this on a regular basis, they are probably sleep deprived and not getting a proper night’s rest.
- Not getting ‘good quality sleep: When you get enough sleep, you’ll wake up refreshed and ready to take on the day. If you don’t get enough sleep, wake up frequently, or have highly restless sleep, you may not get the rest you need.
- Having seizures at night: At night, people may be awakened by seizures, or their sleep may be disrupted so that they do not receive a decent night’s rest. Their brains may be losing out on some of the crucial slumber periods. As a result, a person who suffers from frequent nighttime seizures may find it difficult to operate throughout the daytime. They may also be sleep-deprived and have more seizures during the day!
- Difficulty falling asleep: Inability to fall asleep, frequent awakenings, or waking up too early are all possible causes of sleep disorders. All kinds of things, from mood swings to the negative effects of medication, can cause insomnia.
- Moods: Depression and anxiety can cause sleep problems. If you’ve been experiencing sleep issues for more than two weeks, or if you’ve noticed other signs of depression, it’s time to consult your doctor or mental health professional.
- Poor eating habits: Poor sleep can be caused by a variety of bad eating habits, such as eating too close to bedtime, overindulging in caffeinated beverages like coffee, or consuming alcohol late at night..
- Side effects of medications: Sleepiness is a side effect of some seizure medicines. Other people can make it more difficult to drift off to sleep. Taking seizure drugs at different times of the day may potentially have an impact.
- Sleep disorders: People who have sleep apnea, restless legs, or other sleep disorders may have trouble falling asleep. People who suffer from sleep disorders are more prone to fatigue and sleep deprivation over time. Many people who suffer from seizures also suffer from sleep difficulties.
How Can I Help Improve My Sleep?
- Regularly work out. Examine the form and frequency of your workouts. The best time to get in a good workout is in the morning.
- Do not engage in activities that will keep you awake in your bed, such as reading or watching TV.
- Make sure you have a peaceful and dark place to rest your head before you go to bed.
- Consistency in the sleep schedule is key. To get the most out of your day, stick to a consistent wake-up hour.
- Before you go to sleep, make sure you’re exercising at the right time, eating at the right time, and turning off your electronic devices!
- Allow at least six hours between the last caffeine intake and the time you plan on going to bed. Don’t consume too much alcohol at night.
- Shower before bedtime to help you wind down.
- Don’t work or engage in stimulating activities in the hours leading up to your scheduled bedtime. Instead, engage in activities that promote relaxation.
- Before going to bed, try some sort of soothing exercise, such as meditation.
- After 30 minutes, get out of bed and do something soothing or quiet for around 20 to 30 minutes until you’re ready for bed again. Don’t get sucked into your favorite book! Instead, read something short, like a magazine article, like this one. Go to bed if you’re exhausted. After 30 minutes, if you still can’t sleep, get up. Sleeping in a bed will eventually become second nature to your body.
- Sleep and Epilepsy provide additional advice.
Can Sleeping Pills Help With Sleep?
Over-the-counter sleep aids like melatonin and diphenhydramine may be safe solutions if behavioral techniques fail. A doctor should be consulted before using any kind of sleeping drug (over-the-counter or prescription). Over the course of two or three weeks, do not take sleeping drugs. Even if just in use for a brief time, extreme caution must be exercised. Some persons may get seizures if they discontinue taking benzodiazepines such as triazolam (Halcion), clonazepam (Klonopin), and temazepam (Restoril).
The judicious use of sleeping medications for several nights during a stressful moment, such as the loss of a job or a relationship, can help prevent seizures induced by sleep deprivation. Consult your epilepsy doctor if you find yourself in this circumstance.
But I Just Can’t Sleep Without Sleeping Pills!
If you take sleeping drugs on a regular basis, it’s time to talk to your doctor about the possibility of quitting. Your doctor will most likely begin by gradually reducing the dosage you’re taking. It is possible that he or she will prescribe a sleep aid that is not habit-forming. The doctor may prescribe a medication to treat the underlying cause of the patient’s sleep issues.
Do The Same “Rules” Of Sleep Apply For Children?
Adults need less sleep than children, but children need more sleep than adults. At different ages, the pediatrician can assist you in determining how much sleep your child may require. Additionally, they can assist you in learning more about typical sleep issues in children and how to help them sleep better.
For children who have nighttime seizures or are more exhausted than usual during the day, see an epilepsy doctor. Sleep deprivation can cause seizures in children, so if your child gets more of them when he or she isn’t getting enough sleep, you should make an effort to improve their sleeping habits and stay away from any sleep deprivation triggers.
Nguồn: https://www.sleepyheadpillowcase.com
Danh mục: Best Pillow Reviews